The Unwelcome Guest on Your Skin: Is Psoriasis the Culprit?
Discover the Invisible Triggers and Life-Altering Solutions for This Relentless Skin Condition
Ever noticed those spotty skin patches that appear to come and go? They can be red, scaly, and downright annoying. You might have tried all kinds of lotions and potions to get rid of them, but nothing seems to work. My friend, it's possible that you have psoriasis.
Psoriasis is like that annoying friend who constantly drops by uninvited and stays too long. It affects millions of people worldwide and can seriously lower your self-confidence and self-esteem. But fear not! Knowing what psoriasis is, what causes it, and how to treat and manage it can make a huge difference.
What is Psoriasis?
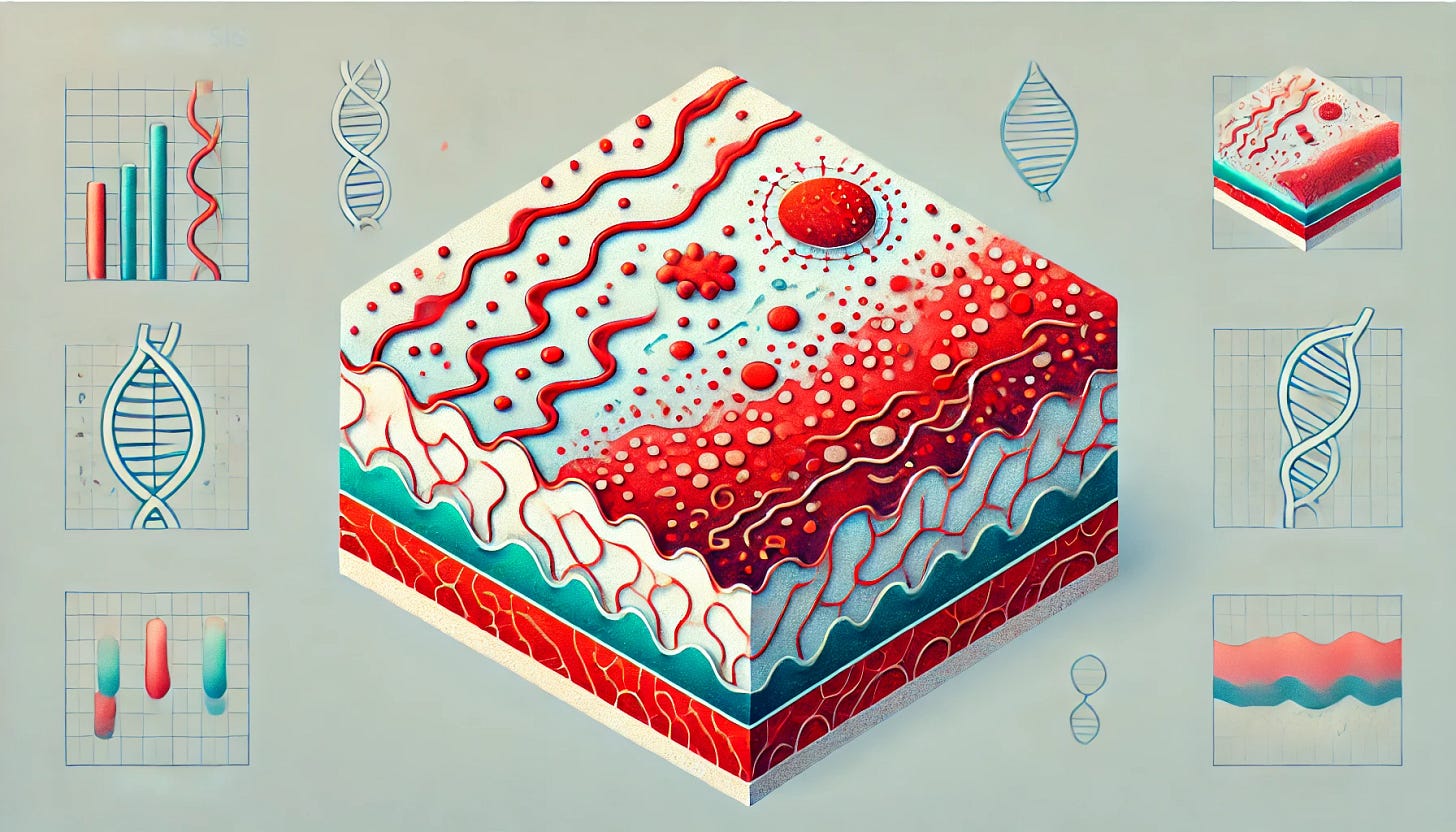
Psoriasis is a chronic autoimmune disease that affects the skin, nails, and joints. It’s characterized by red, scaly spots that can be very unpleasant and uncomfortable. Psoriasis occurs when the immune system mistakenly attacks healthy skin cells, causing them to grow and divide too quickly. This leads to the accumulation of these skin cells, forming the scaly patches associated with the condition.
Varying Incidence Rates Across the World
The prevalence of psoriasis varies worldwide, from 0.09% in Africa to 11.4% in Europe, with a global prevalence estimated at 2.5%. In India, a meta-analysis of 52 studies estimated the overall prevalence to be between 0.44% and 2.8%, with higher rates in northern and western regions compared to southern and eastern areas.
The Red Flags
Skin Lesions: Red, scaly, and elevated lesions that can occur anywhere on the body, often itchy or painful.
Plaques: The most common type of psoriasis lesion, characterized by raised, scaly patches that are silver or red in color.
Nail Changes: Thickening, discoloration, and pitting of the nails.
Joint Discomfort: Pain, stiffness, and swelling in the joints, known as psoriatic arthritis.
Itching and Burning: Psoriasis lesions can be particularly itchy and painful, especially in sensitive areas like the face, genitals, or skin folds.
Dry Skin: Psoriasis can cause dry, cracked skin that is prone to bleeding.
Scalp Involvement: Red, scaly spots, and peeling on the scalp.
What Puts You at Risk?
Psoriasis is influenced by a combination of genetic, environmental, and lifestyle factors.
Genetics: A family history of psoriasis is a significant risk factor. Genome-wide scans have identified a major locus on chromosome 6 (PSORS1) within the major histocompatibility complex, which contains several immune-related genes. Up to 40% of those with psoriasis have a familial history of the disorder.
Environmental Triggers: Air pollution, smoking, infections, stress, and cold weather can trigger psoriasis in genetically predisposed individuals.
Obesity: Obesity is a major risk factor, especially in women. Body fat is inflammatory, producing pro-inflammatory cytokines and chemokines that can contribute to psoriasis.
Medications: Certain drugs, such as lithium, beta-blockers, and antimalarials, can trigger psoriasis.
Vitamin D Deficiency: Vitamin D is crucial for immune system and skin health. Lower levels of vitamin D are often found in people with psoriasis, and supplementation may help improve symptoms.
Hypertension: High blood pressure is linked to endothelial dysfunction and chronic inflammation, both of which can exacerbate psoriasis.
Infections: Streptococcal infections are known to trigger guttate psoriasis, which can recur if the infection is reactivated.
Conventional vs. Functional Medicine: Treatment Approaches
Conventional Treatment: Psoriasis is often treated with a combination of medications, and self-care techniques. For mild to moderate psoriasis, topical therapies such as corticosteroids, vitamin D analogues, and retinoids are common. Phototherapy, or light therapy, is another option, exposing the skin to UV radiation to reduce inflammation and slow skin cell proliferation.
Functional Medicine: This approach focuses on reversing chronic illnesses by identifying and addressing the root causes. For psoriasis, it involves eliminating inflammatory foods, treating gut dysbiosis, healing the gut, addressing hormone imbalances and nutritional deficiencies. Regularly checking micronutrient levels and maintaining a healthy diet can make a significant difference.
Lifestyle Changes and Self-Care
Maintain a Healthy Weight: Obesity can exacerbate psoriasis, so losing weight can help alleviate symptoms.
Avoid Triggers: Identify and avoid triggers that worsen your symptoms, such dairy, gluten, smoking, and certain medications.
Exercise Regularly: Exercise reduces inflammation, improves cardiovascular health, and helps manage stress, which is a common trigger for psoriasis flare-ups.
Stress Management: Practice relaxation techniques like deep breathing, meditation, or yoga to manage stress.
Protect Your Skin: Avoid skin trauma by wearing protective clothing and using sunscreen to prevent sunburn.
Regular Bathing and Moisturizing: Maintain hygiene and avoid harsh soaps and detergents.
Supplements: Krill oil supplements can aid in the healing process, and oregano oil.
Conclusion
Managing psoriasis requires a multifaceted approach that addresses both the physical and mental aspects of the disease. With the right treatment and care, many people with psoriasis can experience significant improvement or even complete reversal of the condition. Always consult with a healthcare specialist to develop a customized treatment plan that is safe and effective for you.